
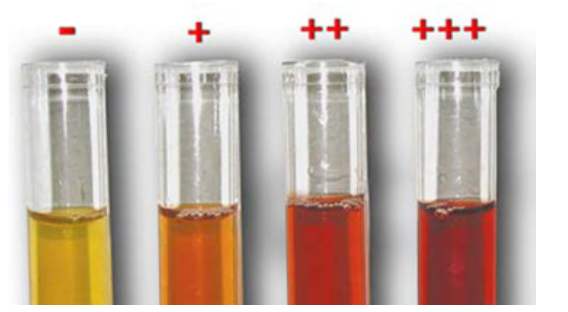
Haemolysis is the leakage of haemoglobin from erythrocytes into the plasma or serum. Haemolysis can occur in vivo with intravascular haemolysis, due to venepuncture technique, or in vitro with inappropriate sample storage or handling. Multiple analytes may be impacted by haemolysis, particularly CK, AST, GGT, phosphorus and calcium. The more severe the haemolysis, the greater likelihood of assay interference.
Haemolysis can be minimised by following the steps below:
• Collect a fasted sample to avoid lipaemia (if clinically possible).
• Select the largest suitable vein and ensure any disinfectant alcohol has evaporated.
• Use an appropriately sized needle and syringe for the vein and consider using a vacutainer.
• Have a clean venepuncture with minimal probing and avoid strong suction on the syringe.
• Collect the blood samples in the correct order.
• Thoroughly mix the tubes containing anti-coagulant.
• Refrigerate the blood samples before submission to the laboratory and ensure the samples remain cool during transport.
• Do not place the tubes directly against an ice pack.
• For chemistry and endocrine tests, centrifuge the sample and remove the serum from the erythrocytes if there will be a delay in submission.
Lipaemia is the presence of elevated triglycerides in the blood. This can occur post-prandially, can be breed associated or can be secondary to disease (eg pancreatitis or metabolic diseases). Lipaemia often results in in vitro haemolysis, further impacting the accuracy of the results. Analytes affected by lipaemia include bilirubin, protein and electrolytes. Lipaemia can be minimised by fasting the patient before blood collection.

Filling blood tubes in this order prevents contamination of serum with EDTA or fluoride oxalate, and minimises activation of the coagulation factors in the sample placed in the citrate tube.
To access the current Order of Draw, scan the QR code below:
